Dosage Calculation RN Critical Care Proctored Assessment 3.1 is a crucial aspect of providing safe and effective medication administration in critical care settings. Understanding the principles, preparation, and strategies for success in this assessment is paramount for nurses to ensure accurate dosage calculation and optimal patient outcomes.
This comprehensive guide delves into the complexities of dosage calculation in critical care, exploring the significance of precision, the intricacies of Proctored Assessment 3.1, and the clinical applications and best practices that underpin medication safety.
1. Dosage Calculation for Critical Care Patients
Accurate dosage calculation is crucial in critical care settings, where precise medication administration is essential for patient safety and recovery.
Commonly used medications in critical care include:
- Vasopressors (e.g., norepinephrine, vasopressin)
- Sedatives (e.g., propofol, midazolam)
- Antibiotics (e.g., vancomycin, piperacillin-tazobactam)
- Analgesics (e.g., morphine, fentanyl)
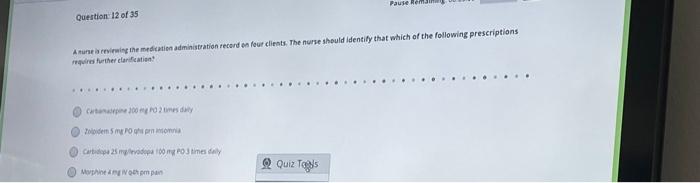
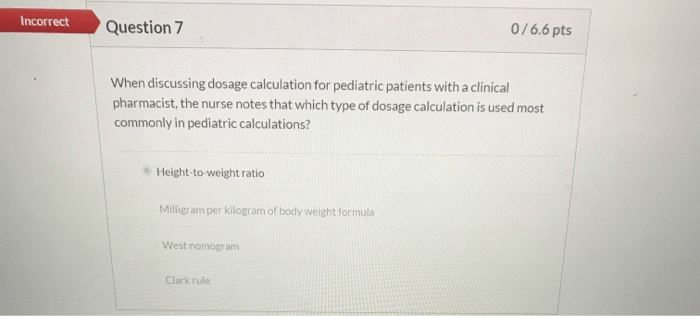
2. Proctored Assessment 3.1
Proctored Assessment 3.1 is a comprehensive evaluation of dosage calculation skills in critical care nursing.
Preparation includes:
- Reviewing medication administration principles
- Practicing dosage calculations
- Familiarizing oneself with the assessment format
Strategies for success include:
- Using the correct formula and units
- Double-checking calculations
- Understanding the clinical significance of the medication
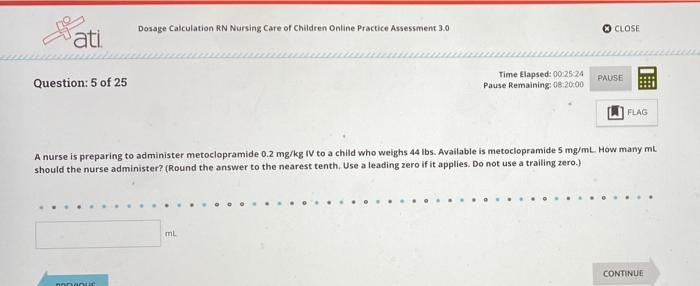
3. Clinical Applications of Dosage Calculation
Accurate dosage calculation ensures safe and effective medication administration in critical care.
Case study:
A patient with septic shock requires norepinephrine. The physician orders a dose of 0.5 mcg/kg/min. The patient weighs 80 kg.
Dosage calculation:
0.5 mcg/kg/min x 80 kg = 40 mcg/min
This calculation ensures the patient receives the correct dose of norepinephrine, which is essential for maintaining blood pressure and organ perfusion.
4. Best Practices for Dosage Calculation: Dosage Calculation Rn Critical Care Proctored Assessment 3.1
| Medication Type | Calculation Method | Verification Process | Potential Errors |
|---|---|---|---|
| IV Medications | Weight-based or body surface area | Double-check calculations, use a calculator | Incorrect weight or BSA, decimal point errors |
| Inotropes/Vasopressors | Titration based on patient response | Monitor patient closely, consult with physician | Overdosage, underdosage |
| Antibiotics | Infection site, severity | Check patient’s renal function, monitor for adverse effects | Incorrect dosing interval, incorrect route of administration |
5. Technology and Dosage Calculation
Electronic health records (EHRs) and other software can enhance dosage calculation accuracy and efficiency.
Benefits include:
- Automated calculations
- Dose range checks
- Medication history tracking
Limitations include:
- Reliance on accurate data entry
- Potential for system errors
Question & Answer Hub
What is the purpose of Proctored Assessment 3.1?
Proctored Assessment 3.1 is a standardized evaluation that assesses nurses’ competency in calculating medication dosages in critical care settings.
How do I prepare for Proctored Assessment 3.1?
Preparation involves reviewing dosage calculation principles, practicing calculations, and understanding the assessment format.
What are some strategies for success in Proctored Assessment 3.1?
Strategies include thorough preparation, time management, and seeking clarification when needed.
